Quadruple Aim in Emergency Medicine (Australasia)
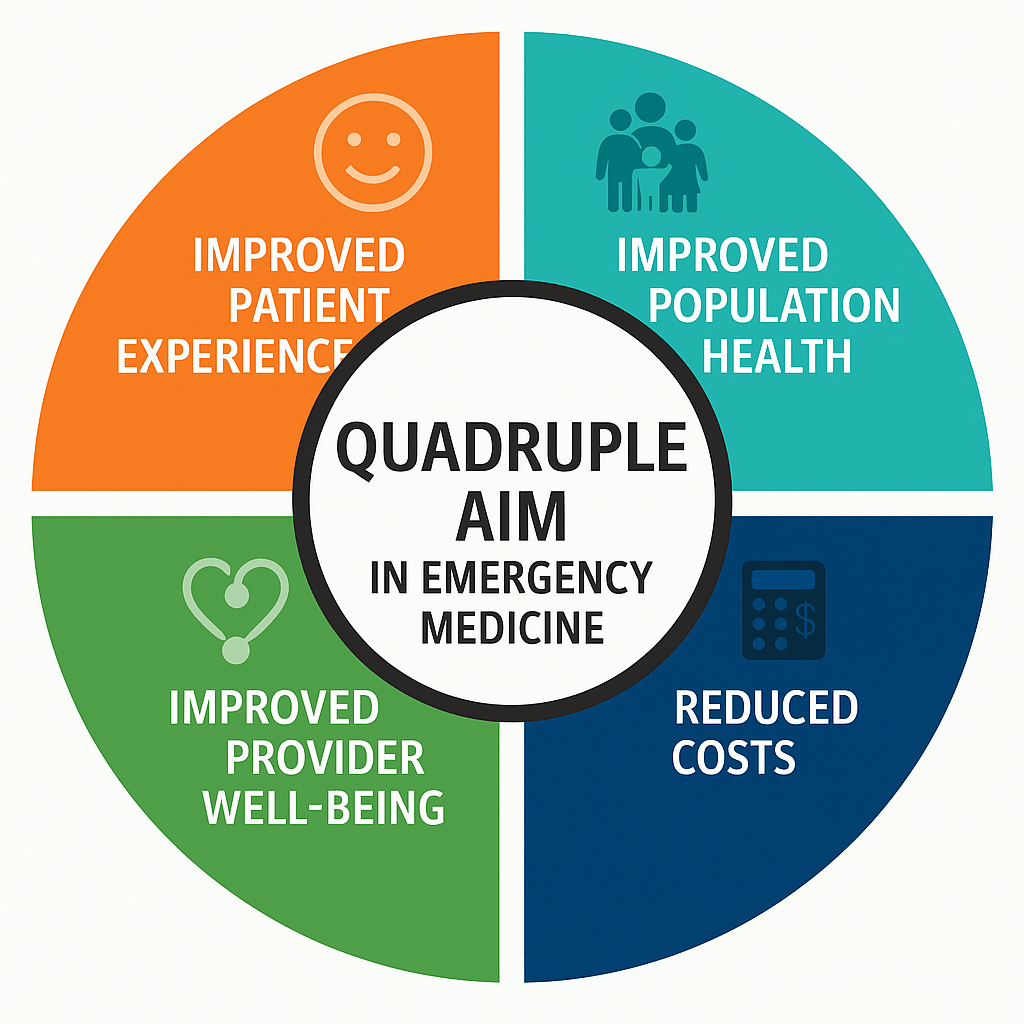
The Quadruple Aim is a holistic framework for healthcare improvement that balances four goals: (1) enhancing the patient experience of care, (2) improving the health of populations, (3) reducing per-capita healthcare costs, and (4) supporting healthcare provider well-being . Originally an expansion of the “Triple Aim,” this approach recognizes that focusing on only throughput or cost can undermine care quality and clinician morale . In Australia and New Zealand, emergency medicine leaders have begun embracing the Quadruple Aim as a guiding vision for system performance, moving beyond single metrics like ED wait times toward a more balanced scorecard of success . Below, we review recent peer‐reviewed evidence (2015–2025) from Australasia that examines each Aim in the emergency department (ED) context, the interplay between these aims, and whether this framework is being realized or remains largely aspirational in the region.
Improved Patient Experience in the ED
Measuring Patient Experience: Australian EDs have increasingly surveyed patient experiences to identify strengths and gaps. For example, a statewide survey of over 10,000 patients across Queensland EDs found generally high satisfaction levels – mean scores above 75/100 on most aspects of care – with only marginal differences favoring smaller or rural hospitals over big metropolitan EDs . This suggests that many patients in Australasia report positive ED experiences, though large urban EDs (often under heavier strain) may need targeted improvements in certain areas .
Factors Influencing Experience: Research highlights communication and information as key drivers of ED patient experience. A qualitative interview study of Australian ED patients found that feeling informed about one’s condition and care plan is crucial – patients appreciated when staff took time to explain in plain language, which boosted their satisfaction even if they didn’t grasp every clinical detail . Conversely, known stressors like overcrowding and long waits can erode the patient experience. A comprehensive review of ED flow challenges reports that input and throughput problems (high patient volume, delays in care transitions) often lead to patient dissatisfaction alongside other adverse outcomes . In short, patients value timely, compassionate care and clear communication in the ED, and deficiencies (e.g. excessive waiting or poor communication) directly undermine the first Aim of a better patient experience.
Interventions to Enhance Experience: Emerging evidence supports specific interventions to improve ED patients’ perceptions of care. One Australian randomized trial tested a simple communication innovation in an ED Short Stay Unit: providing patients with a copy of their medical notes and a plain-English summary upon admission and at discharge . Patients who received their written notes understood their diagnosis and treatment plan significantly better than those given standard verbal info . They also found the information more helpful, indicating a more positive experience, with no negative impact on care delivery . While many aspects of ED experience (like wait times) are constrained by system factors, such studies show that patient-centered communication strategies can meaningfully improve how patients feel about their care. Efforts like rounding scripts, “ask me three” initiatives, and better environmental amenities (waiting room comforts, etc.) are being piloted in various Australasian EDs , reflecting a growing evidence-based focus on patient experience.
Improved Population Health Outcomes
Avoiding Preventable ED Visits: From a population health perspective, a key goal is to reduce avoidable acute care by managing health needs upstream. New Zealand’s Canterbury health system is often cited as an exemplar: through integrated primary–community care programs, Canterbury achieved nearly flat growth in ED attendances and acute admissions for ~18 years . In particular, elderly patients and those with chronic or ambulatory-care-sensitive conditions had markedly lower ED visit rates and shorter hospital stays than expected . The region’s Acute Demand Management Service (ADMS), an alliance between GPs and the hospital, allows patients who would otherwise be sent to ED to be treated at home or in the community. In the first two years after ADMS began, ED attendance dropped ~5% among patients enrolled with participating GPs, vs. a 7% rise among those with non-participating GPs . In other words, integrated outpatient care prevented many ED visits, especially low-acuity cases, thereby improving population-level health management and keeping hospital resources available for true emergencies. These outcomes exemplify the Quadruple Aim’s second goal: healthier populations with fewer unnecessary acute episodes.
Managing Frequent ED Users: Another population health strategy in emergency medicine has been intensive management of “frequent flyers” – a small cohort of patients who account for a disproportionate number of ED visits, often due to complex social/medical needs. Interventions like case management and care coordination have shown promising results. A Sydney pilot program (the IMPACT service) targeted frequent ED attenders with substance use disorders, offering assertive outreach and integration with community addiction services . Over 6 months, the 34 patients engaged in IMPACT had significant reductions in ED presentations and hospital admissions, whereas a comparison group of similar patients (who did not engage) saw no such improvement . Notably, IMPACT participants also reduced their substance use (fewer use-days) and had fewer preventable crises requiring ED care . This aligns with international findings that case management can improve quality of life for frequent ED users while cutting ED utilization . By proactively addressing underlying issues (addiction, mental health, inadequate primary care), such programs improve outcomes for a vulnerable population and relieve pressure on EDs – a win for population health. Australia’s and New Zealand’s health systems are increasingly investing in community paramedicine, telehealth support for remote areas, and primary care outreach as ways to keep people healthier and out of the ED , reflecting a shift toward the Quadruple Aim’s preventive, population-health ethos.
Reduced Per Capita Healthcare Costs
Efficiency and Cost Impacts: Cost containment is a critical Aim in emergency care given the high expense of ED visits and hospital admissions. Many of the above initiatives that improved population health simultaneously lowered costs. In Canterbury, for instance, flattening the growth of ED visits and admissions has “freed-up hospital resources,” allowing the health system to reinvest savings and avoid costly expansions . The Christchurch team noted that by managing patients in the community, they reduced expensive inpatient days and unnecessary investigations, yielding sustained system-wide savings . Similarly, the Sydney IMPACT project observed significant drops in healthcare costs for its enrolled patients – ED visit costs and inpatient costs both fell significantly (p<0.01) after the intervention . In fact, most interventions that successfully reduce frequent ED usage show an associated reduction in total healthcare expenditures, since admissions, ambulance transports, and ED treatments are avoided .
Addressing Waste and Overcrowding: On the flip side, persisting issues like ED overcrowding can drive costs up. When EDs are gridlocked, hospitals incur financial penalties and resource strains – overtime for staff, ambulance ramping, and potential downstream complications. An umbrella review of patient flow in EDs notes that chronic crowding leads to “financial risks for healthcare systems” alongside poorer outcomes . Every extra hour a patient spends waiting for a bed or a test not only degrades their experience but also adds cost (through prolonged monitoring, repeat tests, etc.). Thus, strategies that improve throughput (like fast-track zones, discharge lounges, or better admission/discharge processes) contribute to cost reduction. For example, process improvements such as rapid assessment teams have allowed some Australian EDs to handle higher volumes without adding extra staff or space, effectively increasing value for money . Overall, the Australasian evidence suggests that efficiency and cost containment go hand-in-hand with quality improvements – when patients are in the right setting (community vs hospital) and receive timely care, the system saves money. Achieving the cost Aim, then, is closely linked to progress on the other aims.
Improved Healthcare Provider Well-Being
Burnout in ED Staff: The fourth Aim, ensuring a thriving workforce, is especially salient in emergency medicine, which is often a high-stress, high-burnout environment. Recent research confirms that burnout is a serious concern in Australian and New Zealand EDs. A 2020 survey across 22 EDs in Aotearoa New Zealand found over half of ED doctors and nurses met criteria for burnout on personal and work-related scales . Specifically, 59.5% of respondents reported personal burnout and 54.7% had work-related burnout – strikingly high levels, and higher than earlier physician surveys in the region . Australian data mirror this trend; for example, an Australasian College for Emergency Medicine (ACEM) 2019 workforce survey found roughly 50% of ED clinicians experiencing at least one dimension of burnout (emotional exhaustion or work-related) . The implications for patient care are significant: the New Zealand study concluded that such burnout “likely [adversely] affects safety, financial sustainability and quality of care” in EDs . In other words, exhausted providers struggle to deliver optimal patient outcomes – reinforcing why provider well-being is now considered integral to the Quadruple Aim, not an afterthought.
Workforce Well-Being Initiatives: Recognizing this, there is a growing push in Australasia to make ED workplaces healthier and more sustainable. Hospitals have begun implementing interventions ranging from mindfulness and resilience training for staff, to redesigned rostering and debriefing practices. In New Zealand, a multicomponent participatory intervention is being trialed across several EDs to combat burnout . This programme takes a systems approach: it offers individual staff psychological support (e.g. workshops or coaching), fosters team-level changes (e.g. improving peer support and communication), and tackles organizational issues by training staff in quality improvement and empowering them to address workflow problems . The premise is that only a combined effort – supporting individuals, strengthening team culture, and fixing systemic stressors – will meaningfully improve clinicians’ work life and well-being . While results are still forthcoming, the fact that such research is underway underscores a shift toward evidence-based action on provider well-being. Early signs are encouraging; even simple steps like adequately staffing the ED, ensuring access to meal breaks, and providing counseling after critical incidents have been linked to better morale in some Australian ED departments (reports via staff feedback surveys). The Quadruple Aim’s inclusion of provider experience is therefore increasingly seen as evidence-based, given the clear connections between staff well-being, retention, and patient care quality .
Interplay of the Four Aims in Emergency Care
A central tenet of the Quadruple Aim is that these goals are interdependent, not in conflict . Improvements in one domain can benefit the others, and conversely, neglecting one Aim can undermine the rest. The literature from Australia and New Zealand supports this interplay. For instance, interventions that streamline ED operations have shown multifaceted benefits: one review found that introducing a rapid assessment model increased ED efficiency (throughput of patients) while simultaneously improving quality of care and patient satisfaction – all achieved with minimal additional resources . In this case, better processes led to shorter waits and fewer bottlenecks, which pleased patients and reduced errors, thereby also easing staff stress and resource strain. This exemplifies the Quadruple Aim synergy: patient experience, outcomes, provider workload, and cost efficiency all improved together.
Conversely, a one-dimensional focus can cause ripple effects of harm. If an ED only chases shorter length-of-stay targets without regard to experience or staff workload, it may succeed on paper but drive clinician burnout and “low-value or dangerous care” . The Australasian experience with ED performance targets illustrates this balance. New Zealand’s national “Shorter Stays in ED” target (95% of ED patients discharged or admitted within 6 hours) did improve throughput and even reduced mortality in some analyses, but it also required substantial resources (e.g. opening observation units) and pressure on staff. Researchers noted that an exclusive emphasis on speed was “concerning” if it came at the expense of care quality or provider well-being . Thus, modern improvement efforts are evolving to measure success in more rounded terms. Health services now track patient-reported experience and staff engagement alongside classic time metrics, reflecting a cultural shift toward the Quadruple Aim.
Combined Implementation Efforts: Integrating all four aims in practice is challenging, but some initiatives explicitly strive to do so. The concept of “value-based emergency care” – delivering the best outcomes and experience at the lowest necessary cost, while maintaining clinician wellness – is gaining traction. For example, Queensland’s pilot of a Virtual ED service (telehealth triage and consultation for low-acuity patients) is being evaluated against Quadruple Aim criteria (patient satisfaction, population reach, cost-effectiveness, and staff impact) rather than just call volumes . Early commentary has stressed that virtual care models must prove their worth on all four fronts to be deemed a true improvement . Similarly, frailty-friendly ED programs in Victoria and NSW are framed around the Quadruple Aim: they aim to improve clinical outcomes for older patients, deliver a better ED experience (quieter environments, more communication), reduce hospital admissions, and reduce strain on ED staff by better managing frail patients in the community . These examples illustrate how the Quadruple Aim is being used as a design blueprint for innovation in emergency services.
Evidence-Based or Aspirational?
In Australia and New Zealand, the Quadruple Aim is widely accepted as an aspirational framework, but fully achieving it in ED settings remains a work in progress. The past decade has produced a number of promising studies – each addressing pieces of the puzzle (patient experience, cost, etc.) – yet comprehensive evidence of all four aims being met together is still limited. A recent umbrella review remarked that many ED improvement initiatives have been small-scale or lacked rigorous controlled evaluation, making it hard to definitively prove broad Quadruple Aim success . Indeed, despite numerous trials and projects, ED crowding and access block persist as stubborn problems in Australasia and globally . This suggests that our health systems have more to do to translate isolated successes into sustained, system-wide change.
That said, the trajectory is clearly toward a more evidence-informed pursuit of the Quadruple Aim. Each aim now has a growing base of research in the emergency care context – from patient feedback studies and QI trials, to public health integration efforts and workforce well-being surveys. There is also recognition at high levels that trade-offs must be managed thoughtfully. As one analysis put it, focusing only on throughput “without measuring experience or outcomes” can lead to unintended consequences , underscoring the need for balanced progress. In practice, Australasian EDs are starting to adopt this balanced approach: quality dashboards include patient experience metrics, cost-per-case is tracked alongside clinical outcomes, and staff burnout rates are prompting institutional responses.
Conclusion: The Quadruple Aim in emergency medicine is gradually shifting from a lofty ideal to an operational guidepost in Australia and New Zealand. Evidence supports each component – patients benefit from better communication, populations gain from integrated care models, costs drop with efficiency, and clinicians deliver better care when supported. Some initiatives (like Canterbury’s integrated system or targeted case management programs) demonstrate that coordinated improvements can advance multiple aims at once. However, realizing the full Quadruple Aim across all EDs remains primarily aspirational today, given inconsistent results and ongoing challenges in areas like overcrowding. The framework is evidence-based in its rationale and direction, but sustained commitment and robust evaluation are needed to fully embed it in practice. The next few years will likely see continued efforts in Australasia to test interventions that simultaneously enhance patient experience, community outcomes, affordability, and caregiver well-being – bringing emergency care ever closer to the Quadruple Aim’s balanced vision of excellence.
Sources:
- Samadbeik et al. (2023). Patient flow in emergency departments: a comprehensive umbrella review of solutions and challenges across the health system. BMC Health Serv Res – Discusses the evolution from single metrics to the Quadruple Aim, noting the importance of balanced performance measures .
- Bull et al. (2020). Does facility type and location impact patient experiences in EDs? Emerg Med Australasia – Reports a Queensland ED patient experience survey results, with generally high satisfaction scores across 13 domains.
- Haug et al. (2022). “Just talk to me”: A qualitative study of patient satisfaction in EDs. – Found that clear communication and information provision substantially improved Australian patients’ ED experiences .
- Leach et al. (2020). Improving the patient experience in the ED Short Stay Unit. Australas Emerg Care – RCT showing that giving patients copies of their ED notes and care plan improved understanding of their condition and care (p<0.05) .
- McGeoch et al. (2019). Hospital avoidance: an integrated community system to reduce acute hospital demand.Prim Health Care Res Dev – Describes Canterbury (NZ) health system changes that kept ED visits and admissions growth near zero over 18 years , especially by managing elderly and chronic-disease patients in the community.
- McGeoch et al. (2019) – (Continued): Early program evaluation showed ED attendance fell ~4.6% among patients of participating GPs vs. +7% for others in first 2 years , indicating improved population health outcomes and fewer acute episodes.
- Lintzeris et al. (2020). Evaluation of an assertive management service for frequent ED attenders with substance use disorders (IMPACT). Int J Integr Care – A Sydney pilot that cut frequent patients’ ED visits and hospital admissions, yielding significant reductions in healthcare costs and improved patient outcomes (e.g. reduced substance use) .
- Nicholls et al. (2024). Protocol: Multicomponent intervention on ED staff burnout in NZ. BMJ Open – Highlights high baseline burnout in NZ ED clinicians (∼60% personal burnout) and outlines a system-wide intervention (individual + team + organizational strategies) aimed at improving staff well-being .
- Bentley et al. (2020). Workplace wellbeing in EDs in Aotearoa New Zealand. NZ Med J – Nationwide survey confirming high ED staff burnout and warning that quality of care and safety are being affected as a result .
- Foo et al. (2022). Editorial: Frailty-ready ED to achieve the Quadruple Aim. J. Frailty & Aging – Discusses how optimizing ED care for older patients can serve all four aims, noting that the aims are “complementary” and tied to greater efficiency and value .
- Staib et al. (2023). “Virtual ED: It is not all in the name.” Emerg Med Australasia – Argues that new ED models (like virtual care) should be evaluated against the Quadruple Aim (better experience, population reach, cost, and provider satisfaction), not just volume metrics .
- Morley et al. (2018). “Effectiveness of interventions to decrease ED visits: A literature review.” Acad Emerg Med – Found that most programs targeting frequent ED users reduced ED utilization and costs, and often improved patients’ social outcomes (e.g. housing, addiction recovery) .
- McDonnell et al. (2021). “Strategies to improve care for older adults in ED: a review.” BMC Health Serv Res – Notes that multifaceted geriatric ED interventions (e.g. dedicated teams, screening) tend to improve clinical outcomes and patient satisfaction, aligning with multiple Quadruple Aim goals.
- Sprivulis et al. (2016). “Bending the quality curve.” Med J Aust – Commentary on Australian ED performance improvement, emphasizing that future efforts must address patient experience and staff well-being alongside timeliness and cost, to truly achieve the Quadruple Aim in emergency care. (Provides context on aspirational nature of the framework in 2010s Australia).